Diabetic retinopathy is a complication of diabetes in which extended high blood sugar levels cause damage to vessels of the retina. It’s the most common cause of irreversible blindness in working-age Americans and occurs in more than half of all diabetics.
The longer a person lives with diabetes and the less controlled their blood sugar, the more likely they are to develop the condition. Age, diabetes, prior eye surgery and other factors can increase chances of developing the condition.
Symptoms
Diabetic retinopathy may not present with symptoms in early stages and can subsequently cause damage before patients notice symptoms. These symptoms, which can occur in one or both eyes, may include:
- Blurred or double vision
- Difficulty reading
- Spots, commonly called “floaters,” in your vision
- A shadow across the field of vision
- Eye pain or pressure
- Difficulty with color perception
Diagnosis
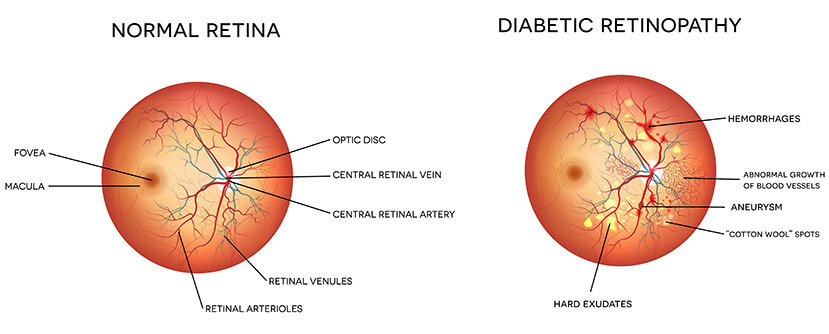
Physicians diagnose diabetic retinopathy with a dilated eye exam. Special eye drops are used to enlarge the pupils allowing a better view inside the eye. A physician will look for swelling of the retina, blood vessel issues indicative of poor circulation, abnormal blood vessels and new blood vessels or scar tissue on the retinal surface.
Other testing can include various types of imaging. Regular exams are important for patients for both prevention and treatment diabetic retinopathy.
Treatment and Prognosis
Several treatments are available for diabetic retinopathy, including small medication injections into the eye, laser treatments, and vitreous and retina surgery. These procedures are designed to prevent, treat, or reverse damage from diabetic retinopathy. Depending on the severity of the condition, your ophthalmologist will discuss the recommended procedures in detail with you.





